ABSTRACT
Edentulism has been demonstrated to have negative social and psychological effects on individuals that include adverse impacts on facial and oral aesthetics, masticatory function and speech abilities, that when combined, are translated into significant reductions in patients’ quality of lives. Full mouth Rehabilitation of patients through implants in areas with severe bone resorption in posterior mandible and maxilla is challenge in implant dentistry. In this context short and bone level implantswiss implants configure treatment option for this type of patient.
Key words: Short implantswiss implants, Bone level implantswiss implants, Marginal bone loss, Mandibular bone atrophy.
INTRODUCTION
Missing teeth have been traditionally replaced with dentures or bridges permitting restoration of chewing function, speech, and aesthetics.1 Dental implants offer an alternative. These implants are inserted into jawbones to support dental prosthesis and are retained because of intimacy of bone growth on to their surface.2
Direct structural and functional connection between living bone and implant surface is termed as osseointegration, first described by Branemark in 19772,3 and has undoubtedly been one of most significant scientific breakthroughs in dentistry over past 30 years.
Very common challenge encountered in use of oral implants is presence of reduced alveolar ridge height is of particular concern when observed in posterior areas of mandible and maxilla, where mandibular nerve and maxillary sinus, respectively, are to be avoided. Aggressive treatment options for reduced alveolar ridge height call for bone grafting area followed by placement of dental implants.4,5 While these methods have obtained level of success, some patients reject multiple surgeries and are discouraged by additional treatment duration date, evidence relating to predictability of surgically increasing vertical ridge height (other than sinus augmentation) is inadequate. At same time, prosthetic solution sometimes is not applicable because of inadequate interarch space.6 An alternative approach in cases where to limited amount of bone height is available is by use short implants of less than 6 mm of length, instead of standard range 10 to 16 mm.7,8 This strategy avoids need for bone augmentation procedures and simplifies treatment.
Implant-supported overdentures and hybrid prosthesis often provide support to soft tissues of face as compared to traditional fixed prosthesis. When adequate number of implants is placed in an arch, conventional fixed bridge is prosthetic modality of choice. In present case we have delivered hybrid prosthesis to patient. Hybrid prostheses’ advantages include decrease in impact force of dynamic occlusal loads, cost-effectiveness, and highly aesthetic restorations. Furthermore, they can be successfully used by a combination of tilted and axially placed implants in partial edentulism in the posterior part of resorbed maxillae.9
The literature regarding the survival of short implants is mixed. Recent clinical studies have demonstrated that short implants may be a viable long-term solution for sites with limited bone height.10 In the last two decades, it became clear that clinical implantology had advanced to the point that this treatment represented a predictable approach to the replacement of lost teeth. These conflicting results suggest the need for additional research efforts aimed at elucidating successful applications and recommendations for the use of short, wide-diameter implants.By placing 4 implant in upper and 4 in lower we could get only 12 teeth support but by placing 6 implant as we have done in our case , we got 14 teeth support.
In this case report we present with, a case of full mouth rehab with atrophic bone manages with placement of short implantswiss implants and hybrid prosthesis in order to gain desired result in a 70-year-old male patient.
CASE REPORT
Diagnosis and Treatment Planning
A 70-year-old patient reported to our clinic, with chief complaint of missing teeth in both upper and lower arches and wanted fixed prosthesis to restore aesthetic and speech. [Figure 1]
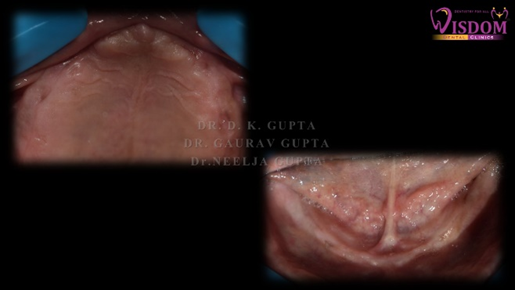
Figure 1: Pre-operative intra-oral photographs
A complete case history was recorded following by thorough intraoral examination. Patient was adviced to undergo routine blood investigation, OPG and CBCT. [Figure 2a,2b]. Going through radiographical and clinical examination full mouth rehabilitation was planned with placement of short and bone level implants with final delivery of hybrid denture in order to get satisfactory results.

Figure 2a: Pre-operative OPG
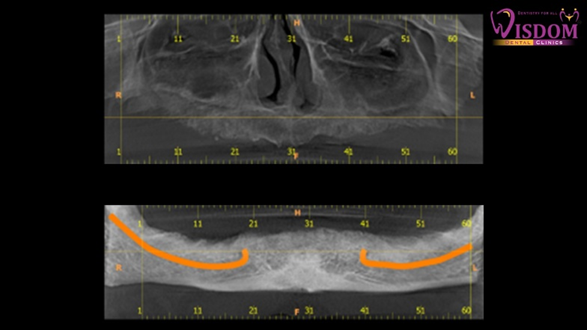
Figure 2b: CBCT
Surgical Phase
Patient was given basic antibiotic and analgesic one hour prior to surgery. Local infiltration of 2% lignocaine with 1:80,000 adrenaline was infiltrated close to the surgical site. Under strict aseptic conditions, a crestal incision was given along the edentulous area all over the maxilla and a mucoperiosteal flap was elevated. Sequential drills were used and implants were placed in the osteotomy site and wrenched into the site until all threads are buried.
Free hand placement of six implantswiss implants was done in the maxilla at canine, premolar and molar site whereas six implantswiss implant were placed in the mandible at canine, premolar, molar site. 3 short implants were placed where bone was deficient in height. Good insertion torque was achieved in the range of 30 Ncm in almost all the implants with ISQ ranging from 74-79. Healing cap was placed. [figure 3]

Figure 3: OPG showing bone level and short implants positioning.
Conventional two-staged approach was followed. Postplacement of implants, the sites were sutured using 3–0 black silk suture. [Figure 4] Postoperative care was administered with antibiotics, analgesics, and mouthwash. Maintenance of oral hygiene and ice pack if needed was suggested.

Figure 4: Suture were placed
After 10 days, the patient was recalled for suture removal. The crestal mucosal showed no abnormal signs.
After 2 months of waiting period, an orthopantomogram was done to ensure the osseointegration. Early loading was planned after 2 months after confirming biological stability, having ISQ in the range of 76-80 throughout. Healing abutment was removed followed by placement of multi -unit abutments placement. [Figure 5]
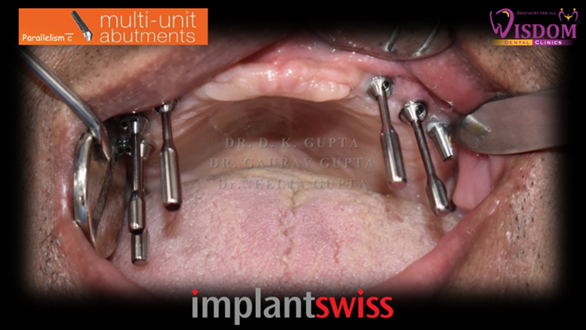
Figure 5: Multi-unit abutment placement
Digital impression of maxillary and mandibular arch was taken after placement of impression copings. Patient was recalled after 2 days for delivery of hybrid denture.
The maxillary and mandibular hybrid prosthesis were fixed along with implant abutments were placed at sites through occlusal screws using torque wrench [Figure 6].

Figure 6: OPG of hybrid denture
Access holes were closed by composite build-up followed by finishing and polishing. Occlusal adjustments were made using articulating paper [Figure7]



Figure 7: Final delivery
The patient was given routine postinsertion instructions for maintenance of oral hygiene. The patient was recalled for review first after a month and then after 6 months.
DISCUSSION
Loss of tooth can be emotionally difficult as it affects speech and masticatory function. Opportunity to achieve better and faster functional results and predictable treatment strategy with very high success rate, has popularized concept of “implant”. Goal of implant dentistry is to provide realistic treatment alternative for patients with tooth loss. Advantages provided by implant supported prosthesis as compared to other conventional treatment options are improved aesthetics, improved hygiene accessibility, osseous preservation and reduced future maintenance.11
Survival rates of short dental implants are quite high, on average 91-97% in patients with generalized aggressive periodontitis and 100% in periodontally healthy patients. Not so long ago, there were restrictions on using short implants associated with its stability and prognosis. However, today, there is an evidence-based scientific basis for effectiveness of use of short implants in rehabilitation of patients with severe ridge atrophy.12 It is often possible not to do additional surgery to augment tissue volume because of design of these implants.13 It is important to note that previously there were age limits, for patients who required implant placement, but at moment, due to technological improvement of method, it is not a contraindication to procedure.14 In our case we too placed short implants which showed successful results in a 70 years old man.
Severe bone atrophy makes doctors apply various augmentation methods, but in some clinical situations, it is necessary to manage only available bone.15 This implies need for a thorough clinical and radiological examination of patient in order to be able to place implants and ensure prosthodontic restoration function, especially if short implants are planned.16
Aesthetic results dependent on marginal bone change over time. Several reports have evaluated the amount of peri-implant bone remodeling over time. These studies have reported radiographic bone remodeling ranging from 0.75 to 1 mm 1st year, with minimal bone remodeling in subsequent years.17 Initial bone remodeling and details of marginal bone change are paramount for predicting stability and location of gingival margin, and are therefore relevant to aesthetic outcome. In recent studies, it was demonstrated that magnitude of initial bone remodeling in patients around 1-piece dental implants was dependent on positioning of rough-smooth border of implant in apico-coronal dimension.18 Bone-level implants take these points into consideration, as different length of healing caps allows user to perform transgingival (1-stage) or subgingival (2-stage) procedure.
In present case we have given full mouth rehabilitation to patient with 6 implantswiss implants in maxilla and 6 implanswiss implants in mandible and hybrid prosthesis in order to gain desired result in a 70-year-old male patient. Rehabilitation of edentulous patients with full-fixed prosthesis has been noticed to achieve greater masticatory function and psychologic satisfaction than with conventional dentures. Occlusal forces following placement of implant-retained prosthesis have been found to have increased considerably.19
CONCLUSION
Oral rehabilitation for partial or fully edentulous dental arches using dental implants and hybrid prosthesis is a remarkable advance in prosthodontics. It is one of the dentistry’s most gratifying treatment modalities, but it demands considerable planning and expertise in addition to a high degree of patient commitment and understanding. Our patient was fully satisfied with the treatment outcome.
REFERENCES
- Wagenberg BD, Ginsburg TR. Immediate implant placement on removal of the natural tooth: retrospective analysis of 1,081 implants. Compendium of Continuing EducDent2001, 22:399-404
- Bajali M., Abdulgani Azz., Abu-Hussein M.; EXTRACTION AND IMMEDIATE IMPLANT PLACEMENT, AND PROVISIONALIZATION WITH TWO YEARS FOLLOW-UP: A CASE REPORT, Int J Dent Health Sci 2014; 1(2): 229-236
- Branemark et al. Osseointegrated implants in the treatment of the edentulous jaw.Experience from a 10-year period. Stockholm: Almqvist & Wiksell Int, 1977.
- Schliephake H, Neukam FW, Wichmann M. Survival analysis of endosseous implants in bone grafts used for the treatment of severe alveolar ridge atrophy. J Oral Maxillofac Surg 1997; 55:1227-1233.
- Bell RB, Blakey GH, White RP, Hillebrand DG, Molina A. Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg 2002; 60:1135-1141.
- Griffin TJ, Cheung WS. The use of short, wide implants in posterior areas with reduced bone height: A retrospective investigation. J Prosthet Dent 2004; 92:139-44.
- Gentile MA, Chuang SK, Dodson TB. Survival estimates and risk factors for failure with 6 x 5.7 mm implants. Int J Oral Maxillofac Implants 2005; 20:930-937.
- Morand M, Irinakis T. The challenge of implant therapy in the posterior maxilla: Providing a rationale for the use of short implants. J Oral Implantol 2007; 33(5): 257-266.
- Kwon T, Bain PA, Levin L. Systematic review of short- (5-10 years) and long-term (10 years or more) survival and success of full-arch fixed dental hybrid prostheses and supporting implants. J Dent. 2014; 42:1228–41. [PubMed] [Google Scholar] [Ref list]
- Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants 2006; 21:275-282.
- Kahnberg KE (2009) Immediate implant placement in fresh extraction sockets. A Clinical report. Int J Oral Maxillofac Implants 24: 282-288.
- M.-S. Howe, W. Keys, and D. Richards, “Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis,” Journal of Dentistry, vol. 84, no. 9, 21 pages, 2019.View at: Publisher Site | Google Scholar
- P. A. Fugazzotto, “Shorter implants in clinical practice: rationale and treatment results,” The International Journal of Oral & Maxillofacial Implants, vol. 23, pp. 487–496, 2008.View at: Google Scholar
- S. R. Schwartz, “Short implants: are they a viable option in implant dentistry?” Dental Clinics, vol. 59, pp. 317–328, 2015.View at: Google Scholar
- V. Pohl, D. S. Thoma, K. Sporniak-Tutak et al., “Short dental implants (6 mm) versus long dental implants (11–15 mm) in combination with sinus floor elevation procedures: 3-year results from a multicentre, randomized, controlled clinical trial,” Journal of Clinical Periodontology, vol. 44, no. 4, pp. 438–445, 2017.View at: Publisher Site | Google Scholar
- U. Lekholm and G. A. Zarb, “Patient selection and preparation,” in Tissue integrated prostheses: osseointegration in clinical dentistry, P. I. Branemark, G. A. Zarb, and T. Albrektsson, Eds., pp. 199–209, Quintessence Publishing Company, Chicago, 1985.View at: Google Scholar
- Pham AN, Fiorellini JP, Paquette D, Williams RC, Weber HP. Longitudinal radiographic study of crestal bone levels adjacent to non-submerged dental implants. J Oral Implantol. 1994;20:26–34. [PubMed] [Google Scholar] [Ref list]
- Ricci G, Aimetti M, Stablum W, Guasti A. Crestal bone resorption 5 years after implant loading: clinical and radiologic results with a 2-stage implant system. Int J Oral Maxillofac Implants. 2004;19:597–602. [PubMed] [Google Scholar] [Ref list]
- Kleis WK, Kämmerer PW, Hartmann S, Al-Nawas B, Wagner W. A comparison of three different attachment systems for mandibular two-implant overdentures: One-year report. Clin Implant Dent Relat Res. 2010;12:209–18. [PubMed] [Google Scholar] [Ref list]
