MANAGEMENT OF IATROGENIC DISPLACED THIRD MOLAR
ROOT WITH LINGUAL PLATE FRACTURE: A CASE REPORT AND
A REVIEW OF TREATMENT APPROACHES
Dr. Gaurav Gupta (Private Practice), Dr. D.K. Gupta (Sr. Consultant), Wisdom Dental Clinics ®, Jaipur, India, Dr. Richa Gupta (Private Practice), The Tooth Clinic, Bareilly, Uttar Pradesh, India
ABSTRACT
The displaced third molar is one of the infrequent but potentially serious complications of extraction. The dental surgeon should localise the tooth fragment by appropriate imaging and should remove it by a technique suited according to the situation. We present diagnosis and management of a case with displaced third molar root in the submandibular space along with lingual plate fracture, root fragment was surgically retrieved without any complications. A review of literature on the present subject is examined and a treatment guideline is suggested for when confronted with such iatrogenic accidents.
Keywords: Iatrogenic displacement of root, lingual plate fracture, third molar, paresthesia
INTRODUCTION
One of the most frequent surgical procedures in oral and maxillofacial surgery is extraction of impacted lower third molar. However, several complications may occur intra-operatively or post-operatively such as: excessive bleeding, tooth fracture, damage to adjacent soft tissues and teeth, bone fracture, displacement of the tooth, paraesthesia of lingual or inferior alveolar nerve, and mandibular dislocation. Accidental displacement of the tooth or its part into adjacent soft tissues is a major complication. Clinically, the individual may observe pain, swelling, trismus, difficulty in swallowing, and respiratory issues.
The most frequent sites of dislodgement are the maxillary sinus and the submandibular space.1 Iatrogenic displacement of maxillary 3rd molars is a rarely reported complication with an unknown incidence. Maxillary 3rd molars have a thin layer of bone posteriorly separating them from the infratemporal space and anteriorly separating them from the maxillary sinus. The tooth can get displaced in a posterosuperior direction in the infratemporal space.2
In the case of a mandibular third molar, the thinness of the lingual cortical bone predisposes to displacement in a lingual direction. Distolingual angulation of the tooth and excessive or uncontrolled force upon luxation are other causes.3
Injury to tissues, pain, swelling, lockjaw, and foreign body reaction are some of the related complications, along with the medical-legal implication.4 Thus, patient history and clinical and radiographic examinations must be rigorously evaluated to establish the best planning of the surgery and avoid the occurrence of accidents and possible surgical complications.
The aim of this current article is to report a case of displaced 3rd molar root with lingual plate fracture and to review the literature on the management of such dental accidents as well as to suggest a rational guideline for its management.
CASE REPORT
A 42-year-old male was referred to the clinic with a displaced root fragment in the left submandibular space; an extraction effort of the impacted lower left third molar was previously attempted elsewhere. Patient’s chief complaint was swelling and tenderness on the left submandibular area commencing 2 weeks ago. He did not have any significant medical history, although mentioned for a previous unsuccessful tooth extraction effort i.rt 3rd third molar few years ago, by his dentist. After doing intraoral examination of the pharyngeal space, a hard tissue mass was palpated below the left medial pterygoid muscle. CBCT computed tomography) revealed #38 (a displaced tooth root) at the left parapharyngeal space and fractured lingual plate. (Figure.1)
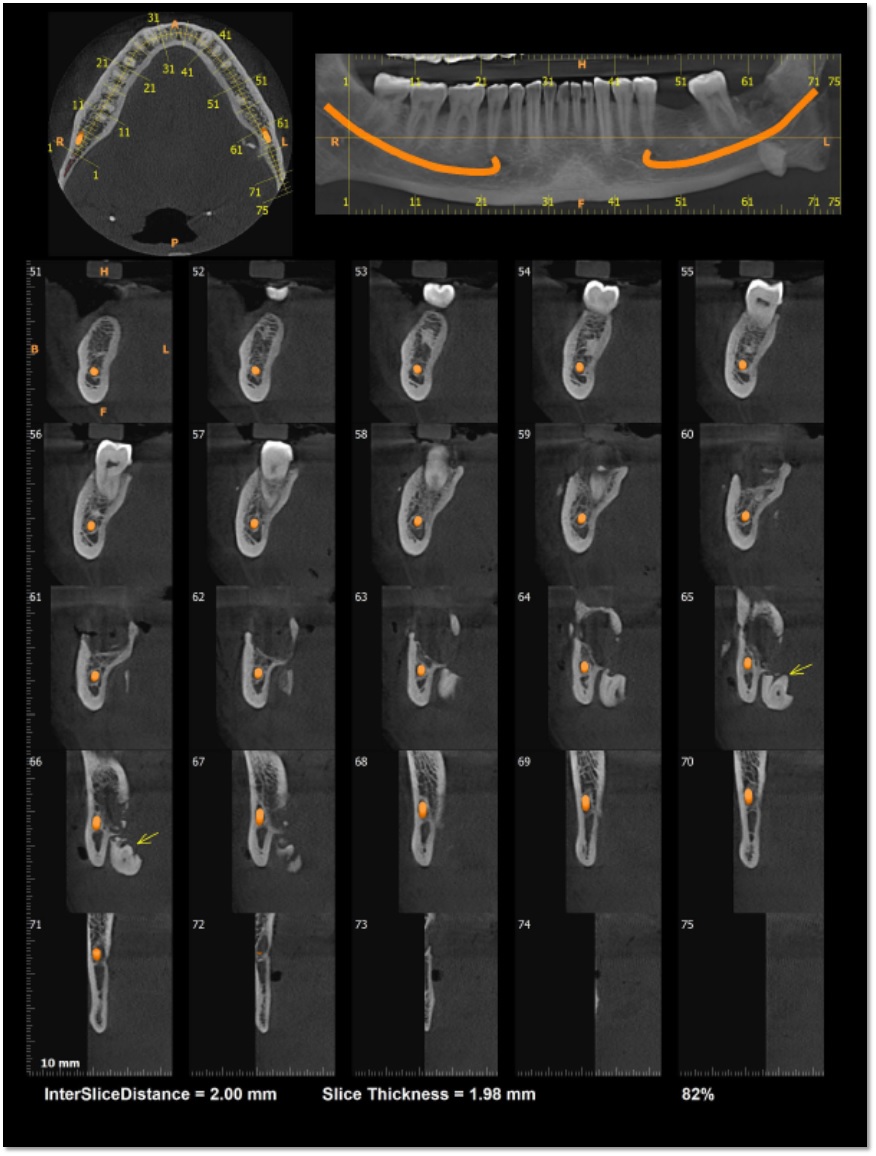
Figure.1 CBCT revealing fractured lingual plate and displaced root i.r.t 38
No clinical symptoms of dysaesthesia of the lip or tongue were present. Informed consent was given to the patient about treatment procedure and patient was prepared for the conservative surgery under local anaesthesia.
A lingual mucoperiosteal flap was raised i.r.t 38 region; an incision was made from the medial aspect of the anterior border of the mandibular ramus, extending up to the lingual gingival sulcus of the mandibular left first premolar. The fractured lingual cortical plate was allowed to remain intact with the lingual mucoperiosteal flap. Blunt dissection was performed medial to the third molar socket area to reach the mylohyoid muscle. The affected tooth was located inferior to the muscle. The tooth was elevated, grasped and removed. Suturing was done to close the elevated flap. (Figure.2)
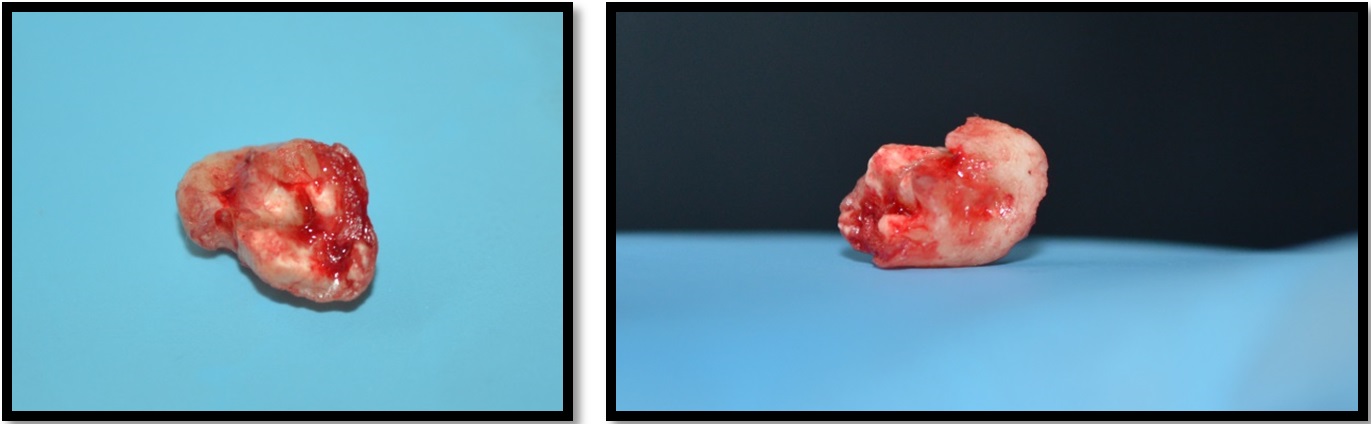
Figure.2a,b Root fragment retrieved during the surgery
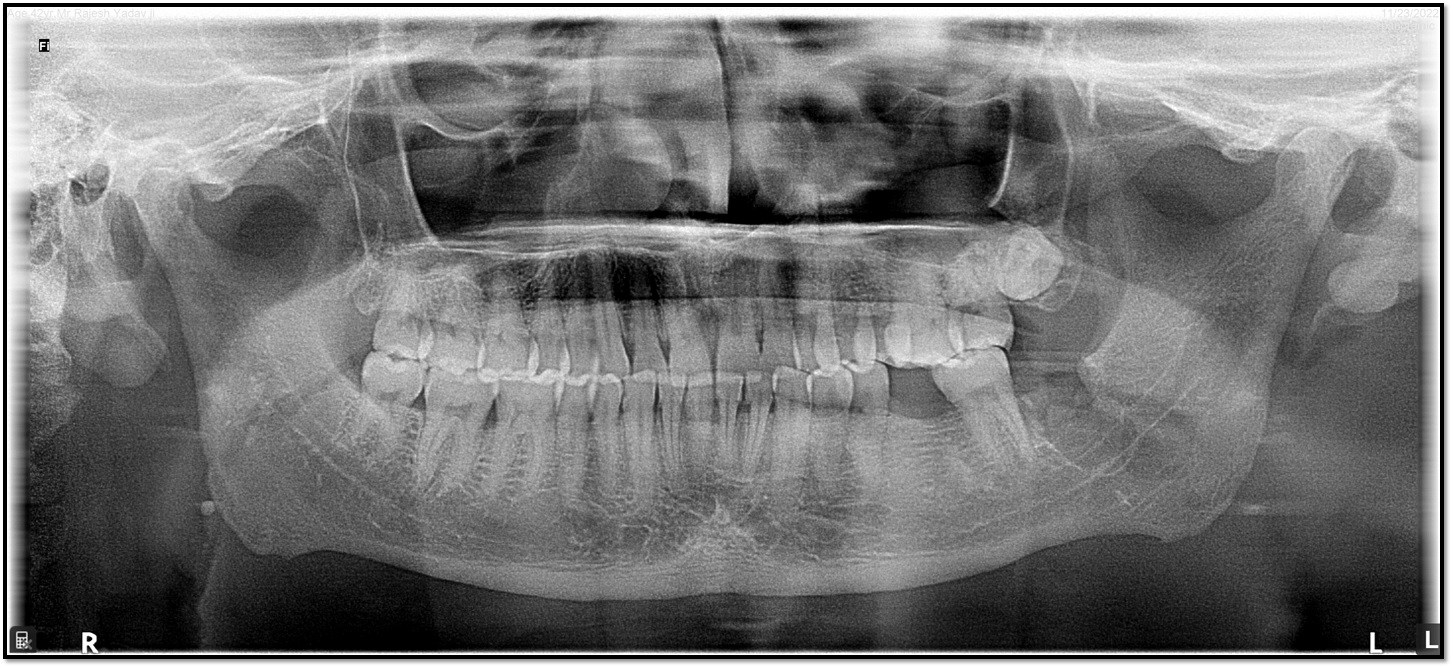
Figure.3 Post-operative OPG
The patient was placed on a week course of analgesic and antibiotic. The patient had normal postoperative healing and was being observed in the follow-up with no postoperative complications. (Figure.3)
DISCUSSION
Accidental displacement of mandibular third molars or their root fragments into adjacent anatomical spaces is a rare yet one of the possible complication.5,6 The estimated incidence rate is <1%. The spaces into which third molars can get displaced are submandibular, sublingual, and lateral pharyngeal spaces.7 This complication occurs due to lingual plate fracture or intraoperative perforation.6 Possible risk factors contributing are thin lingual plate, unnecessary excessive forces applied, incorrect use of surgical instruments or techniques, inclination, and depth of impaction. In the present case root was displaced along with lingual plate fracture.
Displacement of third molars might lead to local infection.6 Furthermore, it is an incidence of great importance due to the proximity of the spaces where the tooth is displaced along with the major anatomic elements of the neck.8,9 Life-threatening complications such as airway obstruction, deep neck infections, erosion of internal jugular vein/carotid artery, and cranial nerve implications may appear.10 Despite of this, it is reported in the literature that many patients are asymptomatic after the tooth displacement. A conservative approach is choice of treatment in such cases.11 Our patient was without symptoms for initial years before he was referred to our department for further management. Thus, we can conclude that there is a wide gap between the time and intensity of symptomatology.
As by our experience gained through this case, it is preferable to retrieve the dislocated teeth/fragments, sooner after the incidence, to avoid the majority of complications. If the patient has symptoms, the immediate removal is of paramount importance.
The efficiency of the treatment relies on the adequate radiographic assessment using OPG imaging / CBCT and CT evaluation when needed which provide a more detailed evaluation of tooth's or fragment's location.8 In the present case too CBCT revealed the actual location of the displaced root with fractured lingual plate and removal of root fragment was planned accordingly.
The timing of fragment's extraction is quite controversial as several surgeons insist on an immediate removal of the residual tooth, while others recommend its extraction after 3–4 weeks of the incident.12,13 The advocates for delay of extraction state that the established fibrosis will ease the fixation of the tooth at its dislocated site, easing its retrieval. However, there might be possible migration of the tooth in a deeper plane and concomitant infection or even airway obstruction.
The surgical approach of tooth's fragment removal is mostly intraoral, while an extraoral or even a combined intraoral/extraoral technique is preferable in some of the cases; for example, when the displaced fragment is located in the lateral pharyngeal or deep cervical space.14 A sagittal split approach is described to the mandibular angle in order to remove a displaced third molar.15 Here we went on with successful retrieval of residual root intraorally and conservative management was done.
CONCLUSION
Adequate clinical, radiological, sound anatomical knowledge and good surgical skills does minimize the chances of complications. CBCT scan is predominant examination in identifying the exact location of the displaced root segment. Proper knowledge of different surgical approaches for the removal of displaced root from the space helps in making the right treatment plan.
REFERENCES
- Pedersen GW. Oral Surgery. Philadelphia: Saunders, 1988:89–90.
- Patel M, Down K. Accidental displacement of impacted maxillary third molars. Br Dent J 1994;177:57–9.
- Huang I-Y, Wu C-W, Worthington P. The displaced lower third molar: a literature review and suggestions for management. Br J Oral Maxillofac Surg 2007;65: 1186–90
- Figueiredo AA, Escoda G. Accidental displacement of third molar roots. J Oral Maxillofac Surg 2012;70:e107-15.
- Lee D, Ishii S, Yakushiji N. Displacement of maxillary third molar into the lateral pharyngeal space. J Oral Maxillofac Surg. 2013;71:1653–7. [PubMed] [Google Scholar] [Ref list]
- Solanki R, Khangwal M, Kumar D, Goel M. Retrieval of mandibular third molar tooth accidentally displaced in submandibular space: Series of two cases. Indian J Dent. 2016;7:105–8. [PMC free article] [PubMed] [Google Scholar] [Ref list]
- Brauer HU. Unusual complications associated with third molar surgery: A systematic review. Quintessence Int. 2009;40:565–72. [PubMed] [Google Scholar] [Ref list]
- Huang IY, Wu CW, Worthington P. The displaced lower third molar: A Literature review and suggestions for management. J Oral Maxillofac Surg. 2007;65:1186–90. [PubMed] [Google Scholar] [Ref list]
- Bouloux GF, Steed MB, Perciaccante VJ. Complications of third molar surgery. Oral Maxillofac Surg Clin North Am. 2007;19:117–28. [PubMed] [Google Scholar] [Ref list]
- Tamer Y, Pektas ZO. Accidental displacement of mandibular third molar roots into the pterygomandibular space. Niger J Clin Pract. 2018;21:1075–7. [PubMed] [Google Scholar] [Ref list]
- Aznar-Arasa L, Figueiredo R, Gay-Escoda C. Iatrogenic displacement of lower third molar roots into the sublingual space: Report of 6 cases. J Oral Maxillofac Surg. 2012;70:e107–15. [PubMed] [Google Scholar] [Ref list]
- Jolly SS, Rattan V, Rai SK. Intraoral management of displaced root into submandibular space under local anaesthesia: A case report and review of literature. [[Last acessed on 2019 Sep 09]];Saudi Dent J. 2014 26:181–4. Available from: http://wwwncbinlmnihgov/pubmed/25382952 . [PMC free article] [PubMed] [Google Scholar] [Ref list]
- Esen E, Aydo?an LB, Akçali MC. Accidental displacement of an impacted mandibular third molar into the lateral pharyngeal space. J Oral Maxillofac Surg. 2000;58:96–7. [PubMed] [Google Scholar] [Ref list]
- Yeh CJ. A simple retrieval technique for accidentally displaced mandibular third molars. J Oral Maxillofac Surg. 2002;60:836–7. [PubMed] [Google Scholar] [Ref list]
- Kontaxis KL, Steinbacher DM. Access to the mandibular angle using a sagittal split to address pathologic displacement of a mandibular third molar. [[Last accessed on 2020 Sep 09]];J Oral Maxillofac Surg. 2015 73:e1-2285-5. Available from: http://dxdoiorg/101016/jjoms201508016 . [PubMed] [Google Scholar] [Ref list]
