PERIPHERAL OSSIFYING FIBROMA: A Case Report
Dr. Nirmala Khanal (P.G Student), Dr. Anuj Gaur (Reader), Dr. Sameeksha Bhardwaj (P.G. Student), Department of Oral Medicine and Radiology, K.D. Dental College and Hospital, Mathura India
ABSTRACT
Peripheral ossifying fibroma (POF) is a localized reactive rather than neoplastic enlargement exclusively on the gingiva. POF has females predominance with site predilection of anterior maxilla in young adults. The absolute diagnosis of such proliferation is histopathological examination due to its variable clinical entity and radiographic characteristics. Here, we report a case of POF in the anterior maxilla in an adult male patient. The existence of such lesion indicates the need of periodontal consultation, and treatment include elimination of subgingival pathology and complete excision of the overgrowth. Long term postoperative follow-up is essential considering recurrence rate of 7-20%.
Keywords : Peripheral ossifying fibroma, reactive, overgrowth, excision
INTRODUCTION
Oral cavity is constantly subjected to various stimuli resulting in numerous localized growths. Among them, gingiva exhibits overgrowth such as pyogenic granuloma, ossifying fibroma, peripheral giant cell granuloma. One such common focal reactive overgrowth with an indolent behavior is ossifying fibroma.1,2 Ossifying fibromas can be central and peripheral. Central type lies in the endosteum or the periodontal ligament adjacent to the apex of the root. Peripheral type arises in relation to the soft tissues in the tooth-bearing areas of the jaws. POF has a peak incidence in young adults, with a predilection for females. Overall, 60% of POFs occur in the maxillary jaw, especially in the incisor-canine region.2,3,4
CASE REPORT
A 18-year-old systemically healty male reported to the Department of Oral and Medicine and Radiology with complaint of a swelling on the left side of his upper jaw since six months. Patient reports progressively increase in size of the lesion without any other associated symptoms that is pain, discharge, bleeding.
Extraoral examination revealed no gross facial asymmetry(Figure 1). Regional lymph nodes were not palpable. Intraoral examination showed a solitary, dome shaped ,pink, sessile, fibrous, exophytic mass extending from 22 to 24 region. Suface ulceration was present on base of lesion (Figure 2).The growth was non-tender and soft to firm in consistency, measuring 1.8 × 1.5 cm in size and protruding from the labial gingiva.

FIGURE 1: Profile of patient : (a) Frontal view; (b) and (c) Lateral view

FIGURE 2: Intraoral view showing the lesion in the left anterior region of the maxilla.
Intra oral peri-apical radiograph revealed opacification of the soft tissues in central area of lower third of root of first premolar on the left anterior maxillary region, with no displacement, resorption of the tooth, or any bone loss in the associated region (Figure 3). Based on the history, clinical presentation, and radiological investigation, the lesion was provisionally diagnosed as POF and planned for oral prophylaxsis and excision under local anesthesia.

FIGURE 3: Intra oral periapical radiograph showing soft tissue opacification in central area of lower third of root of first premolar on the left anterior maxillary region.

FIGURE 4: Excised specimen from the gingiva.
The excised specimen (Figure 5) was sent for histopathological examination. Histology revealed parakeratinized, hyperplastic stratified squamous epithelium overlying a mass of connective tissue stroma. The underlying connective tissue stroma consists of highly cellular mass composed of large number of proliferating fibroblasts, chronic inflammatory cells and numerous blood vessels interspersed throughout the fibrillar stroma. Also, calcifications in the form of irregular bony trabaculae and giant cells interspersed within collagenous stroma confirmed the diagnosis of POF (Figure 5) The surgical site healed satisfactorily with no reported recurrence during six month follow – up(Figure 6).
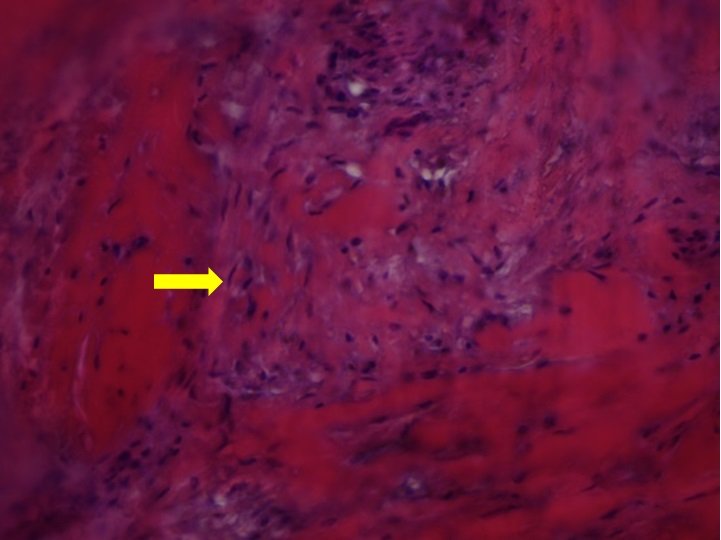
FIGURE 5: Microscopic examination revealing features suggestive of peripheral ossifying fibroma.

FIGURE 6: Post operative photograph after six month of excision of the lesion.
DISCUSSION
Gardner in 1982 coined the term peripheral ossifying fibroma and reinforced as reactive lesion and is not extraosseous complement of central ossifying fibroma of the jaws.5,6 In 90% of gingival biopsies, the connective tissue of the periodontium of the oral cavity can show characteristic localized overgrowths.2,7 Giant cell fibroma, pyogenic granuloma, POF, and giant-cell granuloma are the lesions common in oral cavity. POFs are frequent gingival overgrowths and are also known as ossifying fibroid epulis, peripheral odontogenic fibroma, peripheral cementifying fibroma.8 They occurr due to inflammatory hyperplastic reaction rather than neoplastic. The predisposing factors of POF are oral debris, plaque calculus, ill-fitting dentures, sharp restorations, hormonal change.9 The occurance of POF has been attributed to presence of oxytalan fibers in gingival tissue and progression of pre-existing pyogenic granuloma or a peripheral giant cell granuloma with high potential for the formation of bone and cementum-like materials.2,4
POF is predominat in young adults, with a female predilection. The maxillary jaw, particularly the incisor-canine area, is the site of 60% of POFs overall. Clinically, POF appears as a clearly defined gingival overgrowth that is pink to red in colour with an ulcerated surface. The lesions' bases may be sessile or pedunculated. It generally arises from an interdental papilla with a size of less than 2 cm in its largest dimension and typically does not blanch upon probing.10 Differential diagnosis includes pyogenic granuloma, peripheral odontogenic fibroma, peripheral giant-cell granuloma, fibroma.
These lesions show radiopaque calcifications of soft tissues on radiographic examination, and occasionally there is also accompanying bone damage. The radiographic appearance of tooth migration is only observed in 5% of instances.5 In our patient, intra oral periapical radiograph revealed a soft tissue opacification in the left anterior maxilla; resorption, displacement of the tooth, or any bone loss of invoved site is not associated .Histologically, it appears as a mass of connective tissue made up of cellular fibroblasts and stratified squamous epithelium that is not encapsulated. It occasionally displays an arbitrary distribution of calcifications in the connective tissue, which could result in a false positive diagnosis.11
In order to prevent relapse, the lesion must be completely removed as part of the POF treatment together with all local irritants. Rarely is it necessary to remove the teeth next to the lesion.2 In circumstances when it is left untreated, the lesion may balloon and destroy the bone around it.12 There are reports of these lesions developing in edentulous jaws, despite the fact that the periodontal ligament is where the majority of the POF develops.13 The likelihood of POF recurrence ranges between 8-20%, with the most common causes being incomplete excision of the lesion and aggravating conditions.14 Due to the high likelihood of recurrence of these lesions, ongoing assessment and postoperative monitoring are necessary.
CONCLUSIONS
Since POF shares characteristics with other oral illnesses, diagnosing it can be difficult. For an accurate diagnosis, a thorough clinical and radiographic evaluation in correlation with histological results is necessary. POF should also be taken into account while determining the differential diagnosis of large and acute oral cavity lesions. Complete surgical excision, gingival curettage, and ongoing maintenance of proper dental hygiene are used to treat POFs. Due to the high likelihood of relapse, patients should be monitored for a longer period of time.
REFERENCES
- Kfir Y, Buchner A, Hansen LS: Reactive lesions of the gingiva. A clinicopathological study of 741 cases . J Periodontol. 1980, 51:655-61. 10.1902/jop.1980.51.11.655
- Krishna V K, Periasamy S, Kumar S P, et al. (February 19, 2022) Atypical Presentation of Peripheral Ossifying Fibroma in the Mandible. Cureus 14(2): e22375. DOI 10.7759/cureus.22375
- Katanec T, Budak L, Brajdi? D, Gabri? D: Atypical peripheral ossifying fibroma of the mandible . Dent J (Basel). 2022, 10:9. 10.3390/dj10010009
- Karube, T., Munakata, K., Yamada, Y. et al. Giant peripheral ossifying fibroma with coincidental squamous cell carcinoma: a case report. J Med Case Reports 15, 599 (2021). https://doi.org/10.1186/s13256-021-03187-5
- Sandip Ghosh, et al. Peripheral ossifying fibroma: A case report https://doi.org/10.18231/j.ijpi.2021.031 IP International Journal of Periodontology and Implantology 2021;6(3):179–183
- D G Gardner The peripheral odontogenic fibroma: An attempt at clarification. Oral Surg Oral MedOral Pathol198254140810.1016/0030-4220(82)90415-7
- Kumar SK, Ram S, Jorgensen MG, Shuler CF, Sedghizadeh PP: Multicentric peripheral ossifying fibroma. J Oral Sci. 2006, 48:239-43. 10.2334/josnusd.48.239
- Gardner DG: The peripheral odontogenic fibroma: an attempt at clarification . Oral Surg Oral Med Oral Pathol. 1982, 54:40-8. 10.1016/0030-4220(82)90415-7
- Bodner L, Dayan D: Growth potential of peripheral ossifying fibroma. J Clin Periodontol. 1987, 14:551-4. 10.1111/j.1600-051x.1987.tb00998.x
- García de Marcos JA, García de Marcos MJ, Arroyo Rodríguez S, Chiarri Rodrigo J, Poblet E: Peripheral ossifying fibroma: a clinical and immunohistochemical study of four cases. J Oral Sci. 2010, 52:95-9. 10.2334/josnusd.52.95
- Buchner A, Hansen LS: The histomorphologic spectrum of peripheral ossifying fibroma . Oral Surg Oral Med Oral Pathol. 1987, 63:452-61. 10.1016/0030-4220(87)90258-1
- John RR, Kandasamy S, Achuthan N: Unusually large-sized peripheral ossifying fibroma. Ann Maxillofac Surg. 2016, 6:300-3. 10.4103/2231-0746.200347
- Joshi S, Mazumdar S, Pandit MK: Peripheral ossifying fibroma on edentulous mandibular alveolar mucosa. J Maxillofac Oral Surg. 2015, 14:84-6. 10.1007/s12663-011-0323-9
- Childers EL, Morton I, Fryer CE, Shokrani B: Giant peripheral ossifying fibroma: a case report and clinicopathologic review of 10 cases from the literature. Head Neck Pathol. 2013, 7:356-60. 10.1007/s12105013-0452-1
